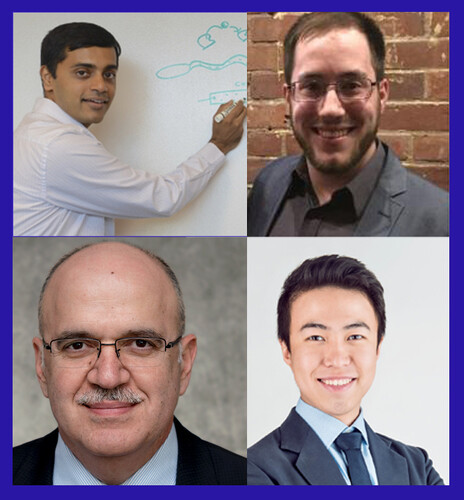
MBB graduate student Peter Dahl and Associate Professor Nikhil Malvankar, PhD, along with other Yale scientists Hao Xing and Themis Kyriakides in Yale School of Medicine, recently published a Scientific Reports study which reveals new insights into the impact of diabetes on fibroblasts, a major cell population that plays a critical role in wound healing. The study, titled “Dysregulation of TSP2-Rac1-WAVE2 axis in diabetic cells leads to cytoskeletal disorganization, increased cell stiffness, and dysfunction,” employed advanced microscopy techniques to investigate various aspects of fibroblast function, including morphology, migration, extracellular matrix (ECM) production, 2D and 3D force generation, and cell stiffness. Dahl and Dr. Malvankar contributed their expertise in atomic force microscopy (AFM) to better understand the elasticity and stiffness of diabetic fibroblasts compared to wild-type fibroblasts.
Some conclusions from this paper showed that diabetic fibroblasts produce a thicker and less porous ECM, which hinders the migration of normal fibroblasts. Migration rate is often correlated with cell stiffness, the Malvankar lab used AFM to probe the elastic modulus (i.e. the resistance of a material to elastic deformation) of the diabetic and wild-type fibroblasts to complement the cell migration assays performed in this study. Diabetic fibroblasts were found to have a slower migration rate, generate less traction force, and have increased cell stiffness- all attributes that could impair wound healing. These changes in fibroblast physiology are likely contributed to a decreased level of the active form of the protein Rac1 and a lack of co-localization between F-actin and WAVE2.
However, the researchers from Kyriakides lab also discovered that deleting the protein thrombospondin-2 (TSP2), another protein important for skin homeostasis and wound healing, in diabetic fibroblasts restored normal levels of active Rac1 and WAVE2-F-actin co-localization and also resulted in the diabetic fibroblasts having a biomechanical phenotype similar to wild-type fibroblasts. These results suggest the regulatory role of the TSP2-Rac1-WAVE2-actin axis and describes a new function of TSP2 in regulating cytoskeleton organization.
The study provides a comprehensive view of the extent of diabetic fibroblast dysfunction and sheds new light on the ways in which diabetes can impact fibroblast function which is critical for wound healing. A better understanding of diabetes and its molecular impacts can lead to new treatments and therapies for patients impacted by this condition.
Congratulations to Prof. Themis Kyriakides, Prof. Nikhil Malvankar, Hao Xing, Peter Dahl and many other collaborators for their work on this article that provides important new insights into the TSP2-Rac1-WAVE2-actin axis in the regulation of proper fibroblast function.
By Jake Thrasher